A major breakthrough of Artificial Intelligence aka AI in medicine and healthcare is the next big thing to happen (or, rather happening already) that is capable of taking medical prediction, prognosis, diagnosis, and treatment to the next level, and help us shift towards a more efficient preventive care approach in the long run.
Before I jump into outlining the prospects of AI in medicine, lemme talk a bit about AI in general and how are these algorithms considered to be intelligent in the first place!
What is Artificial Intelligence (AI)?
AI refers to the capability inferred to a computer program to mimic human behavior in some way. This aims at making our lives easier by achieving higher precision and speed in massive tiresome computational tasks, and by incorporating smart automation in the workflows.
But, just hard-coded algorithms or fixed, rule-based systems don’t work very well for achieving such goals. The solution turned out to be not just mimicking human behavior but mimicking how humans learn. Here comes the terms “machine learning” and “deep learning”.
Machine learning is a subset of AI, and it consists of the techniques that enable computers to figure out patterns from training datasets and deliver AI applications, capable of analyzing test datasets. Basically, machine learning allows machines to go through a learning process. It does this by developing foundational models to solve problems. The machine learning algorithm alters the model every time it combs through the data and finds new patterns. This approach enables learning and provides increasingly accurate outputs. Machine learning can be achieved through several ways, like supervised, unsupervised, semi-supervised or reinforced learning. I've explained the basic concept of machine learning in a bit more detail in my YouTube video.
You might have come across another term called “deep learning”. Now what the heck is that? Deep learning, meanwhile, is a subset of machine learning that enables computers to solve more complex problems, imitating the workings of the human brain in processing data and creating patterns for use in decision making. The deep learning algorithms are capable of reacting to input data by modifying and adapting themselves gradually over the time. In simple terms, deep learning is all about using neural networks with more neurons, layers, and inter-connectivity. We’re still a long way off from mimicking the human brain in all its complexity, but we’re moving in that direction quite fast.
It’s worth mentioning that AI is not something new. Artificial intelligence as an academic discipline was founded in 1956. The goal then, as now, was to get computers to perform tasks regarded as uniquely human: things that required intelligence. It’s the remarkable progress in the field of AI in the last couple of years that has made these terms more popular recently. Also, research on AI in the field of medicine had started quite a few decades back. Stanford has been doing AI in medicine since the early 80’s and it was one of the first sites to have a supercomputer for AI in medicine. But some factors over the last couple of years has accelerated the advancement in this field quite a lot. Advances in computational power paired with massive amounts of healthcare data in electronic form being generated in healthcare systems has given an incentive and has made it imperative that we have to do something with these data to improve the quality and value of care that we provide.
What makes an Algorithm Intelligent?
Doctors are educated through years of medical schooling, doing assignments and practical exams, receiving grades, and learning from mistakes. Much in the same way, AI algorithms are fed with data to train them, the trained models are run on test data, their performances are graded, and the algorithms learn from the mistakes.
There are many different algorithms that can learn from data. Most applications of AI in medicine read in some type of data, either numerical (such as heart rate or blood pressure) or image-based (such as MRI scans or Images of Biopsy Tissue Samples) as an input, which is typically structured, meaning that each data point has a label or annotation that is recognizable to the algorithm. The algorithms then learn from the data and churn out either a probability or a classification. For example, the actionable result could be the probability of having an arterial clot given heart rate and blood pressure data, or the labeling of an imaged tissue sample as cancerous or non-cancerous. After the algorithm is exposed to enough sets of data points and their labels, the performance is assessed to ensure accuracy, just like exams are conducted to assess medical students. This process involves the input of test data to which programmers already know the results, allowing them to assess the algorithm’s ability to determine the correct result. Based on the performance, the algorithm can be modified, fed more data, or rolled out to be applied in clinical environments.
Approaching ‘Precision Medicine’ through AI
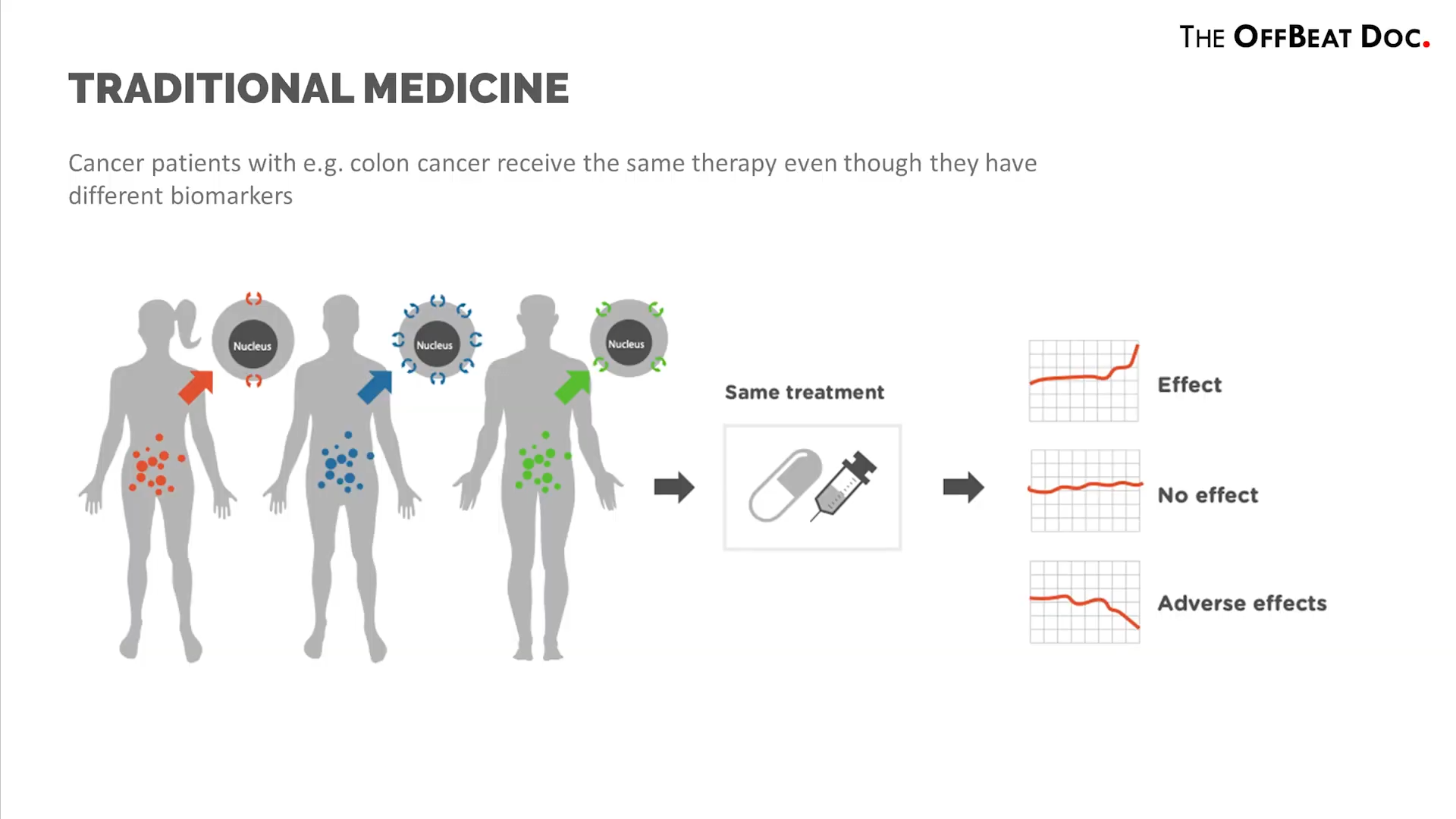
Classical medical practice puts large groups of people in their focus and tries to develop clinical solutions, and hence the treatment protocols or drugs developed thereof are usually based on the needs of the statistical average person.
As everyone has a different genetic code, a different lifestyle, exposed to different environmental conditions and medications, they may react differently to a particular pharmaceutics or may have a completely opposite reaction to treatment as assumed. Here’s where the concept of ‘Precision medicine’ comes into play.
Now, as we are in an age where masses of data can be collected and analyzed very quickly, personalizing treatment can become more feasible by means of machine learning and deep learning AI algorithms. So, AI will most likely help healthcare move from traditional, ‘one-size-fits-all’ medical solutions towards targeted treatments, personalized therapies, and uniquely composed drugs.
For instance let's talk about Cancer diagnosis. It can be immensely complicated for the doctors in making decisions about diagnosing a primary or secondary cancer, also in understanding the risks and success rates of the treatment options.
From Reactive Diagnostic Approach to Predictive Prognosis
Usually patients visit the clinics presenting some signs and symptoms of an acute or chronic disease. The doctor examines the patient and checks lab investigation reports and makes a diagnosis. Based on the diagnosis he follows a treatment strategy. So this is reactive diagnosis, that is the doctor is reacting after the patient presents with the disease.
But consider the scenario where a patient visits for a regular checkup. Now AI algorithms can handle even minute and apparently irrelevant clinical/diagnostic aspects of patients that might predict a disease the individual can contract in maybe 10 years of time. And even if the patient has some disease it can make precise predictions of the possible complications that might occur which might have been impossible for a human.
We can develop and train such AI models based on clinical findings, trends, and outcomes of other patients. Imagine how much more useful it would have been if the doctor could be presented with the patient’s risk for stroke, coronary artery disease, and kidney failure based on the last 50 blood pressure readings, lab test results, race, gender, family history, etc.
All we need is huge sets of databases of patients and development of competent AI algorithms. Already many such AI models have been developed to predict several diseases and healthcare issues with much accuracy, so that the individual can adopt precautionary treatment/lifestyle early enough to avoid falling victim to it in future.
Recently Google's Deepmind has developed an AI technology that has the ability to not only spot deterioration more effectively, but actually predict it before it happens. Their AI model could accurately predict Acute Kidney Injury (AKI) in patients up to 48 hours earlier than it is currently diagnosed. Importantly, the model correctly predicted 9 out of 10 patients whose condition deteriorated so severely that they then required dialysis. This could provide a window in the future for earlier preventative treatment and avoid the need for more invasive procedures like kidney dialysis. The model has also been designed so that it might, in the future, generalise to other major causes of diseases and deterioration such as sepsis, a life-threatening infection.
Use of AI in Drug Development
We can apply AI in diverse sectors of the pharmaceutical industry, including drug discovery and development, drug repurposing, improving pharmaceutical productivity, and clinical trials, among others; such use reduces the human workload as well as achieving targets in a short period of time.
It is worth mentioning about Atomwise, which uses supercomputers that root out therapies from a database of molecular structures. In 2015, Atomwise launched a virtual search for safe, existing medicines that could be redesigned to treat the Ebola virus. They found two drugs predicted by the company’s AI technology which may significantly reduce Ebola infectivity. This analysis, which typically would have taken months or years, was completed in less than one day.
Challenges faced in Developments of AI Solutions in Healthcare
Now it's quite obvious that AI has vast potential in healthcare. but it lags behind other industries by years.
The main factor limiting the usefulness of machine learning is that healthcare data is far more complex than data in other industries, and difficult to aggregate. Machine learning algorithms are only as good as the quantity and quality of data that we feed them. More well-organized the data is, easier for the algorithms to analyze them; and more voluminous the data, more is the accuracy and precision of the trained model.
Advancements in electronic medical records have been remarkable, but the information they provide is not much better than the old paper charts they replaced. If technology is to improve care in the future, then the electronic information provided to doctors needs to be enhanced by the power of analytics and machine learning. We have to use the EHR (Electronic Health Records) from across the different health institutions and convert them into well-organized datasets enabling them to be implemented later in training AI models. But this is by far the biggest challenge in the field of AI in medicine. But thanks to recent EHR standards like FHIR (pronounced “Fire”) being implemented, which can result in better interoperability, availability, and ease of exchange of healthcare data for research purposes in the field of AI.
Like any digital health tool, AI models can be flawed, presenting risks to patient safety. These issues can stem from a variety of factors, including problems with the data used to develop the algorithm, the choices that developers make in building and training the model, and how the AI-enabled program is eventually deployed. Here comes the domain of state laws and regulations.
Moreover, assembling sufficiently large patient datasets for AI-enabled programs can raise complex questions about data privacy and the ownership of personal health data. Protections to ensure that sensitive patient data remains anonymous are vital. However, anonymizing patient data can pose its own challenges, as it can sometimes undermine efforts to ensure the representativeness of large datasets; if patient demographics are unknown to AI developers, then they may not be able to detect bias in the data.
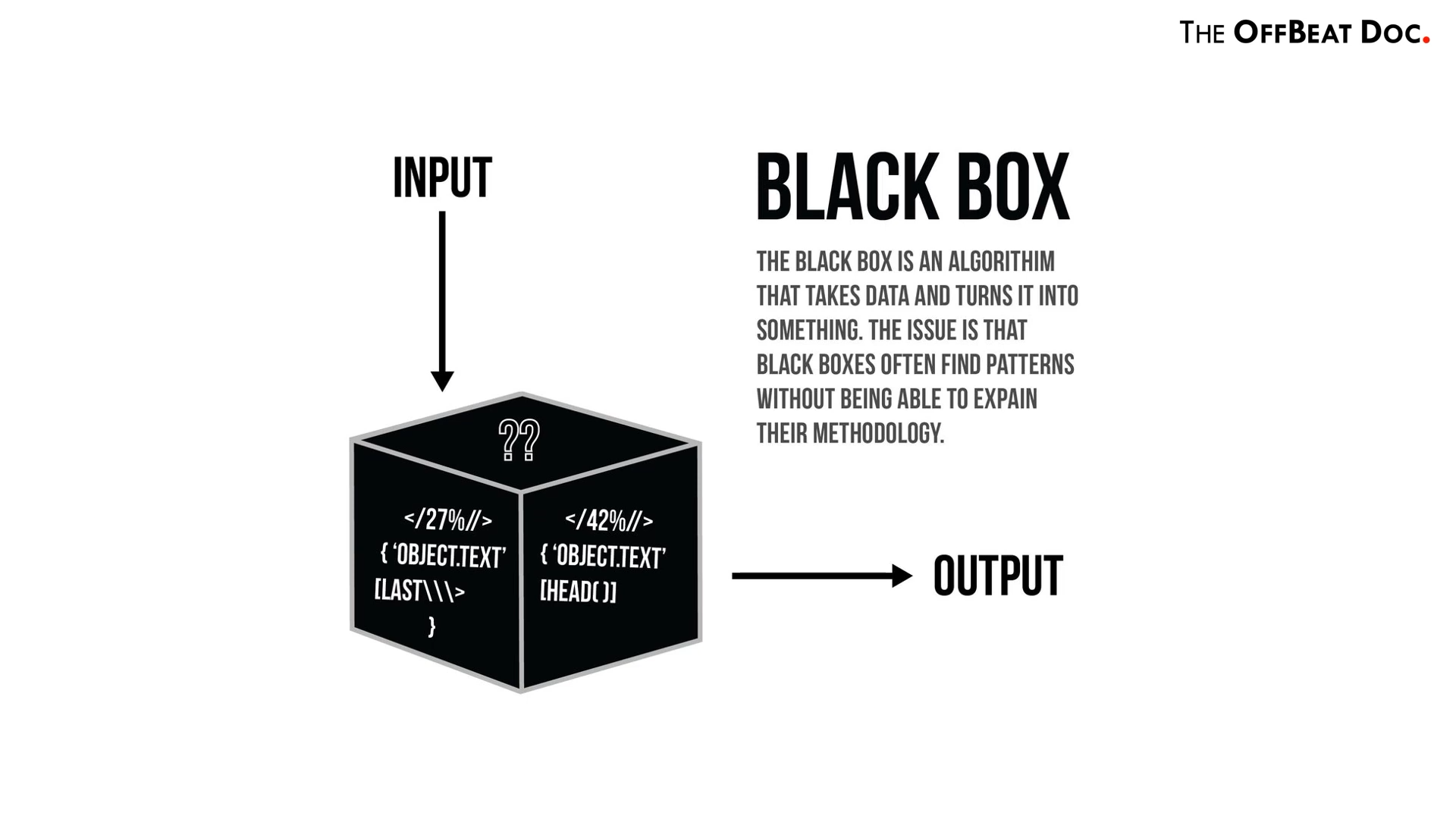
Also the ‘black box’ problem is one of the key barriers for the implementation of AI in clinical practice. The algorithms are derived from large datasets using complex techniques and reflect underlying patterns that may be too convoluted for a person to understand. Hence it might be too difficult to explain to the end user how a program produced a certain result.
What does AI mean for the Future of Doctors?
Will AI replace doctors? LOL, No.
While it’s quite unlikely that machines will replace or eradicate the need for human doctors any time soon, I think, those who are already pursuing or are considering a medical profession should be willing to adapt, learn and grow alongside technological advancements. AI won't replace doctors but doctors who use AI will definitely replace those who don't.
This hybrid model of humans and machines working together creates new tasks and roles for essential medical and technology professionals, increasing the capabilities of the entire field as we move forward.
Conclusion
Thanks for reading through this post. Do let me know what is your opinion regarding the developments and implementation of AI technologies in medicine in the comments section. It’s The OffBeat Doc signing off. ✌

 Listen to this article
Listen to this article.png)